Log in to your PhysioU account and check it out! Don’t already have a PhysioU account? Create a trial account here!
Application
NeuroAnatomy
We are proud to announce our exciting new NeuroAnatomy App.
Intentionally designed with progressively more challenging activities, it provides opportunities for the learner to build a solid foundation of neuroanatomy for clinical practice. Beautiful graphics include an interactive 3D model of the brain and spinal cord, with actual human anatomical slices that are labeled with explanations.
Content expert Charlotte Chatto, PT, Ph.D., Board Certified Clinical Specialist in Neurologic Physical Therapy has had a passion for finding creative ways of teaching neuroanatomy and treating patients with neurologic conditions for over 30 years.
Features:
In the four Neuroanatomy Explorer Challenges, each with multiple sections, practice questions cover basic concepts, structures, functions, and dysfunctions of the brain and spinal cord. Interactive Mini-Games are incorporated into the Challenges to reward the learner with fun facts about the nervous system.
In Learn by Slice, the learner can choose a slice of the brain or spinal cord and explore the major structures on the slice by clicking on anatomical pins to reveal explanations.
In Learn by Tract, the learner can understand connections between anatomical structures, through short explainer videos, overview images, and clickable structures, to reveal the location and function of major motor and sensory tracts.
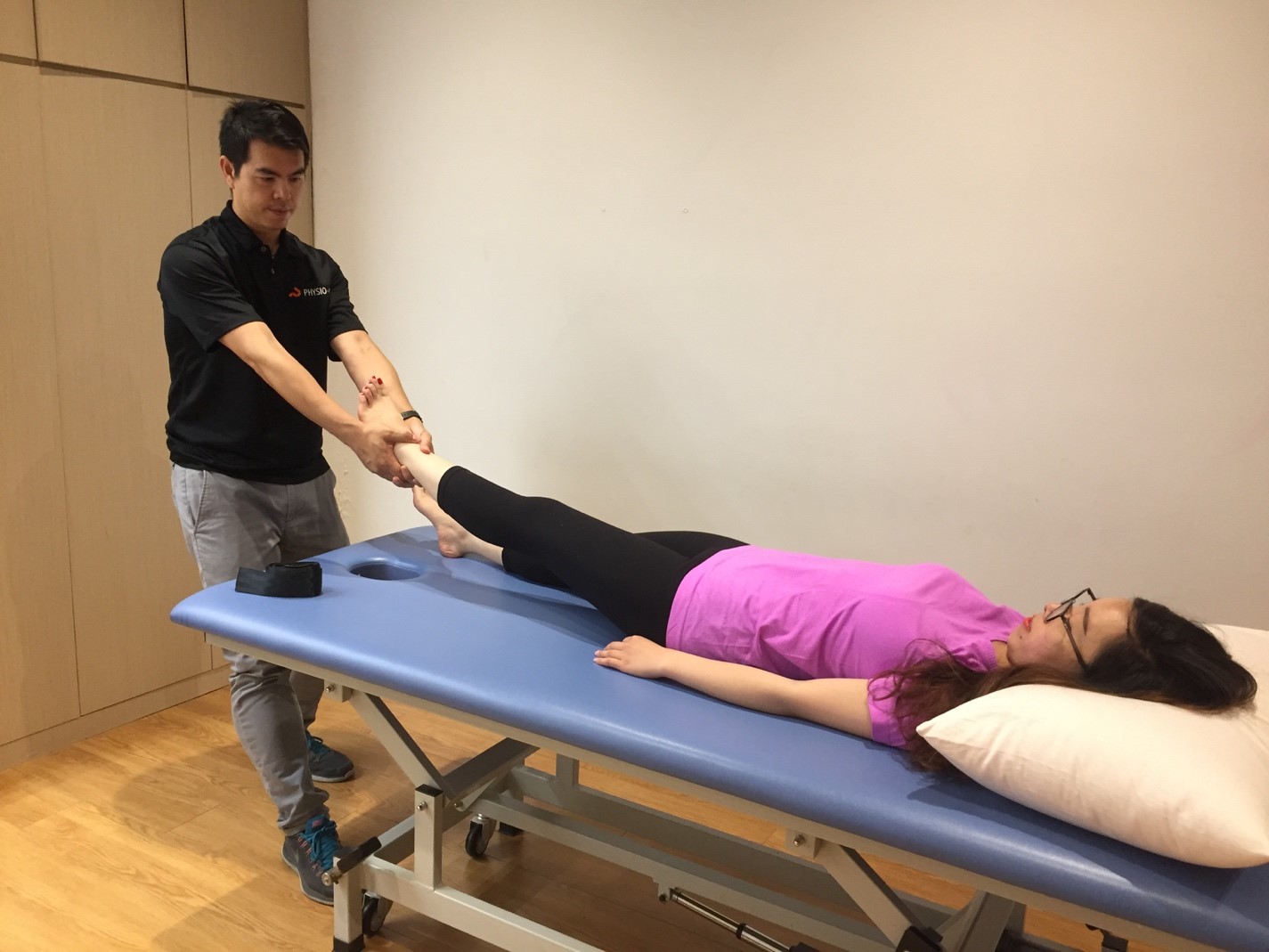
Task Analysis
The Task Analysis App was designed to bring the client into the classroom. Based on the seminal work of Dr. Patty Scheets, PT, MHS, DPT, and Dr. Lois D. Hedman, PT, DScPT, MS, the PhysioU team followed clients into their home setting, capturing glimpses of functional tasks in the context of the clients living environment. Multiple angle video allows for detailed analysis and discussion as young clinicians develop the skill of task and movement analysis.
The app starts with the “Learning” section which includes expert movement analysis and sample documentation of 5 common activities using the 1Hedman movement analysis framework and 2 sample tasks based on 2Scheets Task Analysis by Dr. Mary Hudson-McKinney PT, MS, DPT, NCS:
Scheets Task Analysis:
Quiet sitting
Sit to stand
Hedman Movement Analysis:
Getting out of bed
Toileting
Bringing food to mouth
Quiet sitting
Sit to stand
The clients featured in the app span a spectrum of different genders, ethnicities, and conditions including:
“Typical” male
“Typical” female
Client Post Total Hip Replacement
Client with Congestive Obstructive Pulmonary Disease
Client with C5 Incomplete Spinal Cord Injury
Client Post Cerebrovascular Accident
Each Client was filmed performing a range of activities in their home environment:
Dressing
Grooming
Food preparation
Toileting
Bed mobility
Leisure activities
Driving
Gardening
Case studies and Analysis worksheets are integrated into the app for classroom activities, discussion, and development of activity analysis skills.
Special Acknowledgements:
Special thanks to Dr. Mary Hudson-McKinney PT, MS, DPT, NCS for her contributions to app design and expert analysis/documentation for the Learning section of the app.
Special thanks to all of the clients who invited us into their homes and their lives, so that we could create learning tools to elevate professional education.
Hedman LD, Quinn L, Gill-Body K, Brown DA, Quiben M, Riley N, Scheets PL. White Paper: Movement System Diagnoses in Neurologic Physical Therapy. J Neurol Phys Ther. 2018 Apr;42(2):110-117. doi: 10.1097/NPT.0000000000000215. PMID: 29547486.
Quinn L, Riley N, Tyrell CM, Judd DL, Gill-Body KM, Hedman LD, Packel A, Brown DA, Nabar N, Scheets P. A Framework for Movement Analysis of Tasks: Recommendations From the Academy of Neurologic Physical Therapy's Movement System Task Force. Phys Ther. 2021 Sep 1;101(9):pzab154. doi: 10.1093/ptj/pzab154. PMID: 34160044.
Simulations & e-Learning
Neuro Macro
Clinical reasoning development for neurologic rehabilitation. The PhysioU Team and Dr. Sara Kraft have created interactive learning simulations that cover a comprehensive evaluation and treatment of clients with various neurologic conditions including:
Spinal cord injury case study
Stroke case study
Vestibular case study
Learning objectives for the simulations include:
Interpret information from a subjective examination and apply it to a clinical scenario
Understand the side effects of common medications and how they may affect a physical therapy treatment session
Analyze data from outcome measures to guide clinical decision making
Develop a one hour treatment session to address the impairments discovered throughout the case
These 45-60 minute long simulations are designed to help students apply their knowledge in a context-rich environment. The learning modules help students to connect the dots of examination and interventions. These simulations are typically deployed at the end of the week after the students learn about managing each of the above noted neurologic conditions.
Learn how to assign these simulations in your syllabus here.
Learn how to add videos to lecture and lab here.
Determine how to use the learning reports so that you can track student participation.
Postures
The Posture SIMs were designed to help students further develop their reasoning skills after they have learned the basics related to posture. Simple clinical scenarios have been created so that students can link postural faults to possible impairments of body structure and function. These impairments are then logically connected to interventions, with sample videos (of the techniques) so that students can connect the dots to techniques that they may not yet have learned. These sims are relatively simple and formative in nature.
Best Use Case:
These sims should be used during the week of or after the students learn about postural deviations.
Learn how to assign these simulations in your syllabus here.
Learn how to add videos to lecture and lab here.
Determine how to use the learning reports so that you can track student participation.
Wound Care Marco
Wound care management concepts are difficult for students to wrap their heads around. 9-12 questions (about 5% of the board exams) will cover content related to the integumentary system. The PhysioU team has created interactive clinical reasoning simulations to help students apply the knowledge they have learned in class. In the Wound Care Simulations, there are 5 microlearning emodules that allow students to test their knowledge in the following topics:
Burns
Treatment types
Debridement
Lymphedema
Wound types
The two new release MacroSIMS create a patient centered clinical reasoning development experience that helps students “learn by playing.”
The two MacroSIMS include clients with the following conditions:
Diabetic neuropathy
Venous insufficiency
Special thanks to our wound care specialists who were critical in the creation and vetting of these e-learning modules:
Dr. Jennifer Vicenzo PT, MPH, PhD
Dr. Erin Vogel PT, DPT, OCS, WCC, AIB-PT
Dr. Shelley Swen PT, DPT, CWS, CLT-LANA
CPG Orthopaedic MiniGames
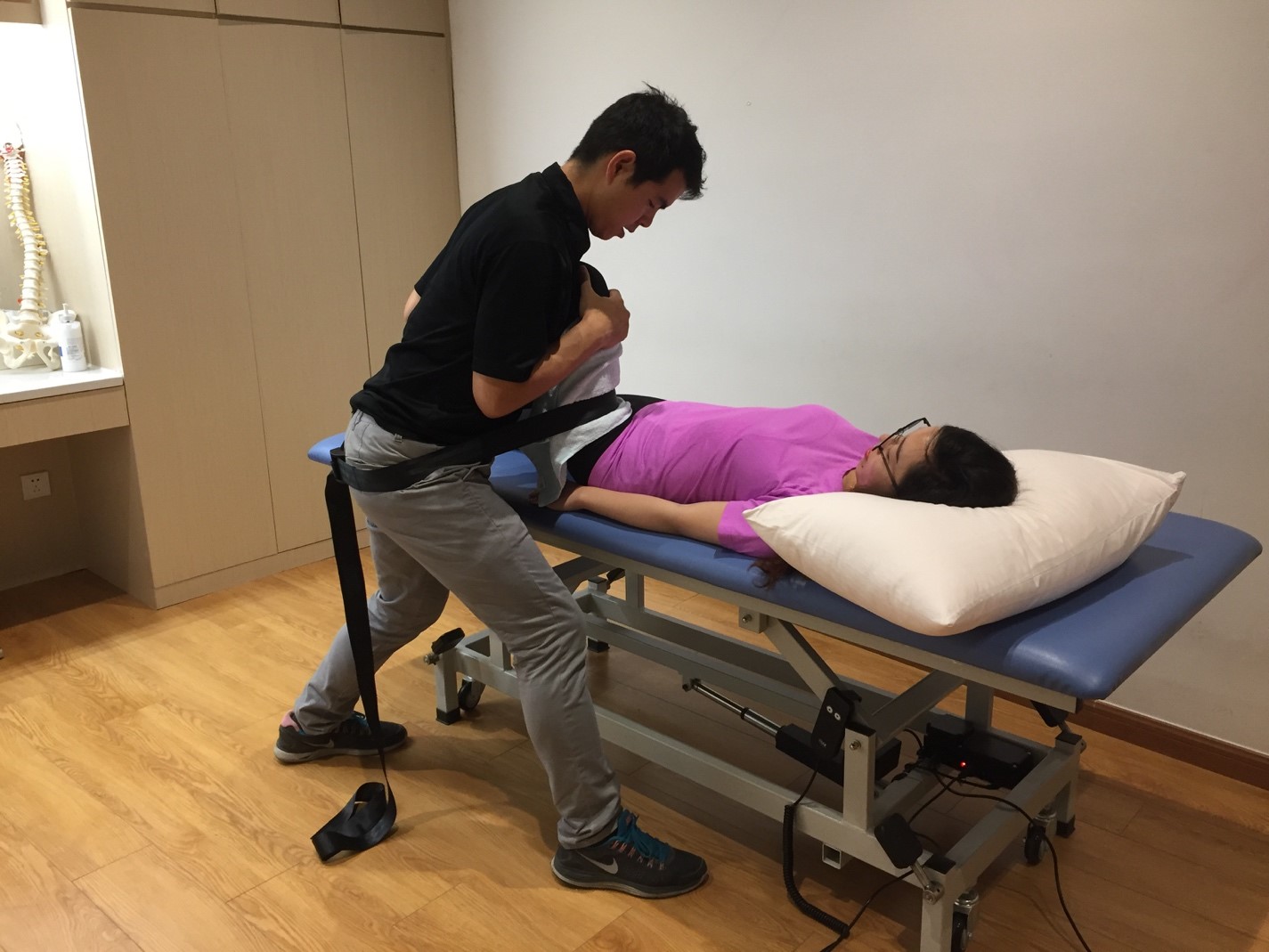
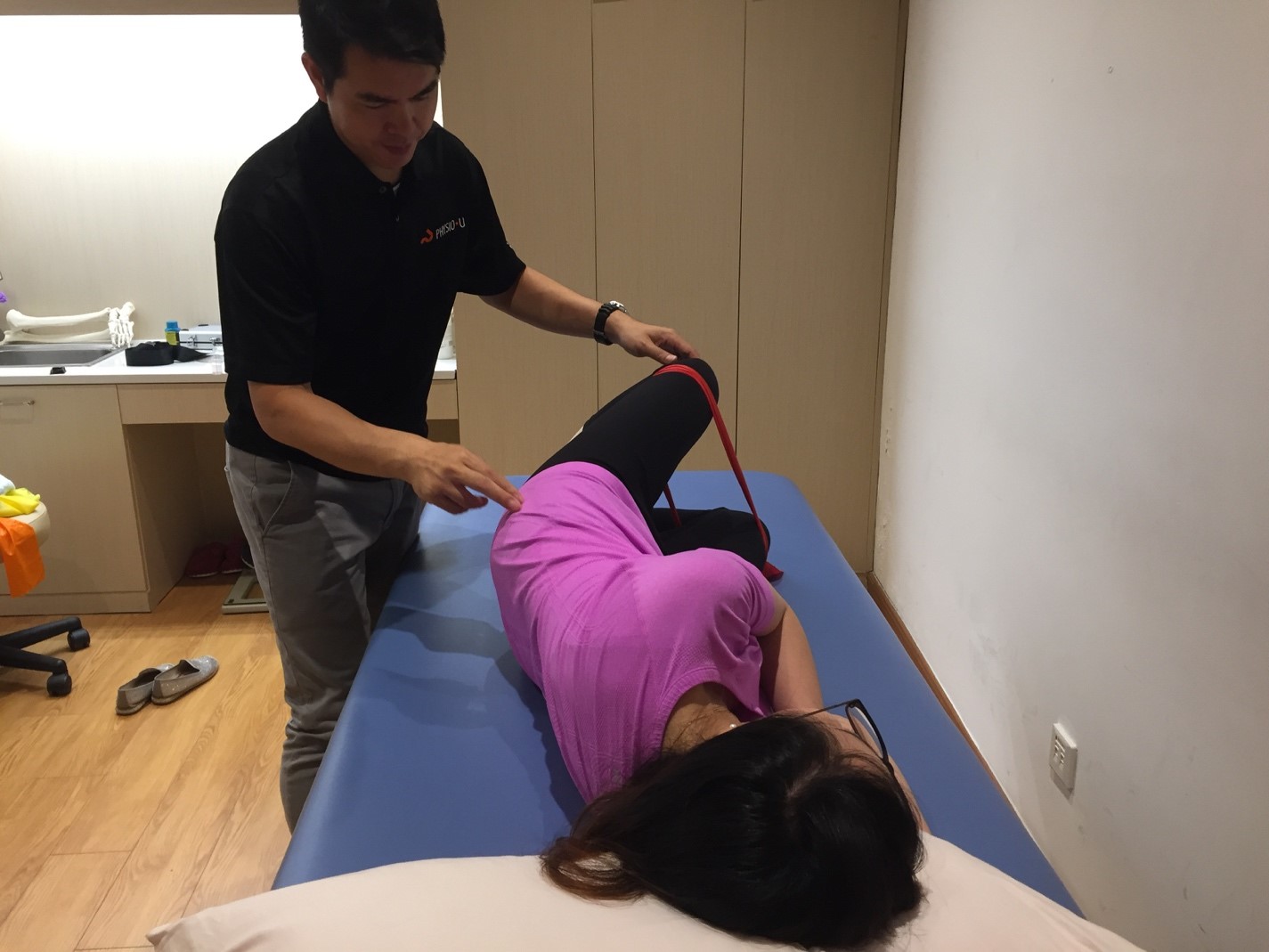
Clinical practice guidelines are gamified! We are proud to announce the new Musculoskeletal Rehabilitation Foundations set of MiniSIMS built exclusively around the practice standard setting guidelines released by the Academy of Orthopaedic Physical Therapy and Journal of Orthopaedic and Sports Physical Therapy (JOSPT). Each MiniSIM is built with the new learner in mind, starting with patient subjective complaints and objective findings that help with clinical pattern recognition. Testing procedures as described by the guidelines are demonstrated using high definition video and interactive matching of interventions to impairments of body structure and function help a student to connect the dots between examination and treatment.
Best Use Case:
These simulations should be used during the week before you teach about a body region (Neck pain/cervical spine, for example) as a scaffolding exercise and the building of clinical patterns for students. They can also be used at the end of a week (after cervical spine week, for example) as a way for the students to connect the dots of all the things that they have learned during that week. These apps were built so that someone with almost no experience can begin their pattern recognition development process.
Learn how to assign these simulations in your syllabus here.
Learn how to add videos to lecture and lab here.
Determine how to use the learning reports so that you can track student participation.