Mid Back Pain with Mobility Deficits
Patients with excessive thoracic spine kyphosis often report diffuse achy pain in the mid thoracic spine; especially with upper trunk extension or extension-rotation movements. It is important to note that mobility deficits in the thoracic region can result in pain in surrounding structures such as the neck, shoulder, or lower back! For more clinical findings click here!
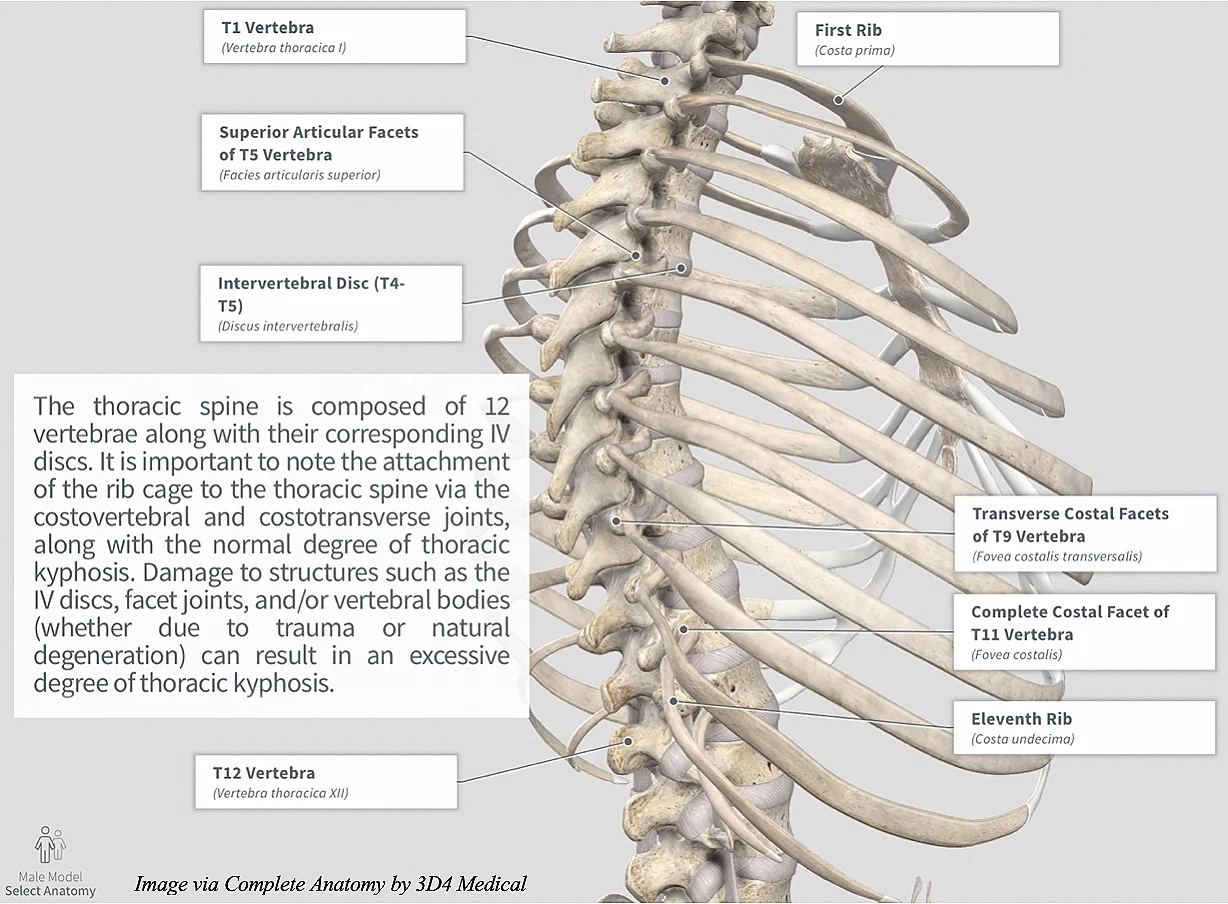
Anatomy
Image via Complete Anatomy by 3D4 Medical
Movement Fault
Although excessive thoracic spine kyphosis can typically be identified in standing and/or seated postural assessments, the quadruped position is an excellent functional alternative to analyzing the thoracic spine and how it’s movement interacts with the rest of the body! (Click image to watch 1-2 minute video)
Key Finding
As mentioned before, patients with mobility deficits of the thoracic spine often experience exacerbation of symptoms with extension and/or extension rotation movements. Be sure to assess the patient’s active range of motion to see which direction they are most limited in! (Click image to watch 1-2 minute video)
Treatment
If the patient is deemed appropriate for manipulative therapy, a high velocity low amplitude thrust (HVLAT) can help provide immediate symptom improvement. (Click image to watch 1-2 minute video)
Therapeutic Exercise
After manual therapy is provided, it is imperative to follow up with therapeutic exercise in order to promote the new movement pattern. Although multiple exercises can help improve thoracic spine extension, it is important to give patients something they can do regularly. Thoracic spine extension over a chair is an exercise that can be performed anywhere! (Click image to watch 1-2 minute video)
As always, address the individual as a whole, determine which are the primary impairments and begin treatment there!